Wounds can result from injuries, surgeries, or medical conditions like diabetes and limited mobility. If you do not receive adequate treatment, your healing process is delayed, or new problems can develop.
Physical therapy supports wound healing and helps reduce the risk of recurrence through techniques that improve circulation, mobility, and pressure relief. You recover safely and regain function with the proper care plan, including movement, positioning, and wound management techniques.
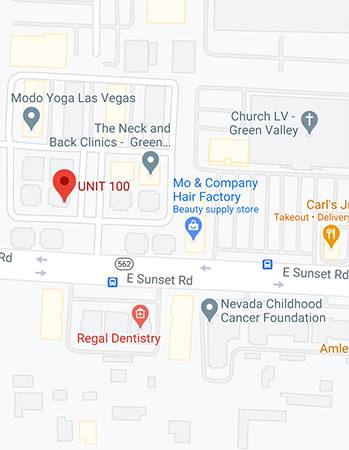
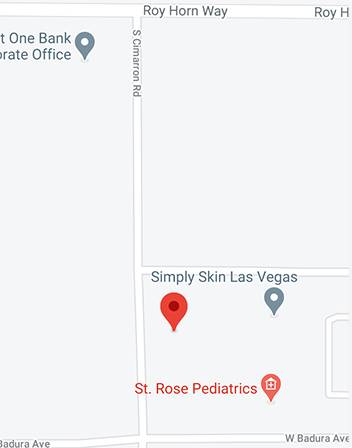
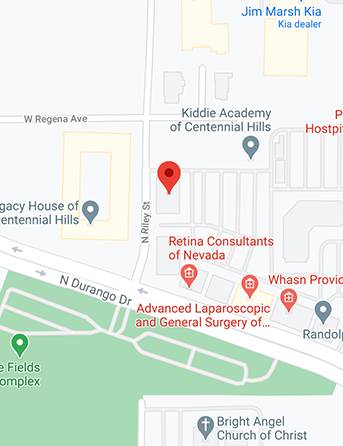
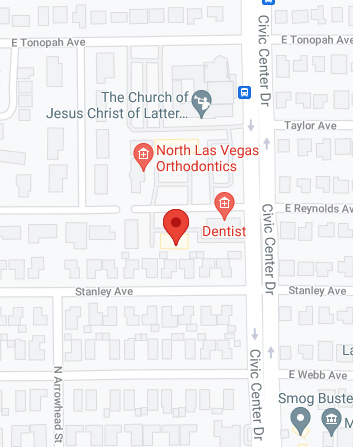
At Suarez Physical Therapy in Las Vegas, our physical therapists are ready to support you with effective, personalized care focused on healing and long-term well-being.
An Overview of Wounds, Who is at Risk, and Their Causes
A wound is any break in the skin or underlying tissues. The skin barrier disruption allows bacteria and other microbes to enter the body. While microbes are commonly found on wounds, their presence ranges from harmless contamination to harmful infection, depending on their behavior and the body’s response. Knowing the stages of microbial activity, contamination, colonization, and infection helps identify when a wound is problematic. The stages include the following:
Contamination
During contamination, the microbes are on the wound, not multiplying or causing harm.
Colonization
During colonization, microbes begin to grow, and while there may be no visible tissue damage, the immune system may still respond subtly to the microbial presence. When microbes multiply rapidly, the immune system weakens, leading to tissue damage and slower healing.
Infection
A body’s inability to manage microbial growth leads to infections. Infection can develop due to multiple factors, including a weakened immune system, high microbial load, and the virulence of the invading organisms.
Initiation of medical care is vital since infections can escalate to skin infection (cellulitis), bone infection (osteomyelitis), and bloodstream infection (sepsis), which potentially result in death or amputation.
Early identification of wound condition helps reduce the risk of infection and supports timely intervention if signs of illness arise. The signs of infections are difficult to detect, particularly in cases of chronic wounds. Expert clinical assessment and proper medical care are essential, especially in light of the growing issue of antibiotic resistance.
Who Is at Higher Risk?
- People with diabetes, poor circulation, or weakened immune systems
- Older adults or those with limited mobility
- Underweight individuals, overweight ones, and those who suffer from dehydration and malnutrition
- Smokers and those on certain medications (like steroids or chemo)
Multiple risk factors may combine, resulting in elevated dangers of developing chronic wounds. The treatment of chronic wounds depends on continuous observation and prompt medical intervention.
Common Types and Causes of Wounds
Several events, including daily mishaps and severe medical conditions, lead to wound formation. Proper treatment and prevention strategies depend on identifying the underlying cause. Common causes include the following:
Accidents and Trauma
Wounds from cuts, scrapes, punctures, or severe injuries caused by falls or machinery accidents are common. Wounds resulting from dirty or sharp objects, bites, or deep and large wounds have a greater chance of infection.
Surgery
Surgical procedures lead to deliberate wounds, but these wounds still carry the potential to become infected. Surgical site infections (SSIs) occur in approximately 2–4% of patients. Various factors, including diabetes, obesity, smoking, extended surgical duration, and weakened immune system function, increase the risk of infection.
Burns
When your skin is damaged by heat, chemical, or electrical burns, it carries a high risk of infection and delayed healing. Improper management of these wounds can result in their developing into long-lasting chronic conditions.
Circulation Problems
Reduced blood flow leads to persistent leg injuries, which become chronic wounds. Peripheral Artery Disease (PAD) leads to arterial ulcers by reducing blood flow and nutrient delivery to tissues, which impairs wound healing and increases tissue breakdown.
Chronic Venous Insufficiency (CVI) develops when damaged leg veins fail to efficiently circulate blood, leading to venous ulcers and leg swelling.
Diabetes
People with diabetes have a higher risk of foot wounds because of these factors:
- Reduced sensation due to neuropathy prevents individuals from noticing injuries
- PAD is prevalent among people with diabetes, and it impairs the healing process
- Diabetes delays healing because of impaired immune response, reduced circulation, and nerve damage that affects tissue repair mechanisms
Immobility and Pressure Injuries
Prolonged sitting in one position causes blood flow to reduce, and this could lead to pressure injuries, also known as bedsores. Patients who remain in bed or use wheelchairs and those who wear casts or oxygen masks often develop pressure injuries.
People with diabetes who have PAD and nerve damage are at a higher risk of developing foot wounds.
Types of Chronic Wounds
Chronic wounds are wounds that do not heal significantly within about four weeks, often due to underlying health issues. Physical therapists handle four distinct types of chronic wounds as part of their treatment practice. These wounds develop because of health issues that affect blood circulation or nerve system integrity and limited body movement. Treatment success depends on recognizing the distinctions between these wounds.
Arterial Wounds (Ischemic Ulcers)
Peripheral Artery Disease (PAD), usually caused by atherosclerosis, reduces blood flow to the extremities. Plaque formation in arteries leads to blockages that stop oxygen and nutrients from reaching the skin. Some of the characteristics of these wounds are
They appear on bony areas like the heels, toes, ankles, and the front of the lower leg. They appear as single, round, punched-out wounds with well-defined borders and pale grey or black inside. The skin around them may be smooth, hairless, feel cold, and appear pale in color. They cause significant pain, especially at night or when elevated.
Their healing is very slow. The recovery process is complicated because of poor blood flow and the risk of developing infections. You are at a high risk of developing gangrene, warranting surgical removal of the affected tissue. Surgical interventions will improve blood flow during treatment.
Diabetic Wounds (Neuropathic Ulcers)
People with diabetes often have nerve damage (neuropathy) and poor circulation due to PAD, both of which impair the body’s ability to heal wounds and fight infection. The heel, ball of the foot, bottom of the foot, and toes are frequent sites where these wounds may develop.
These ulcers typically appear round and are often surrounded by thickened skin (callus), a common characteristic. Depending on its stage and severity, the wound bed may appear pink or have darker pigmentation. You do not feel pain due to nerve damage. Many people only discover foot wounds when they notice drainage or signs of infection.
Healing is difficult due to poor circulation, nerve damage, and a slower immune response. Infected wounds occur often, leading to bone infections and potential amputation risks. You must regularly inspect your feet and wear appropriate shoes to prevent foot issues.
Pressure Injuries (Bedsores)
Pressure injuries develop when prolonged pressure impairs capillary blood flow to the skin and underlying tissues, leading to localized tissue damage. These injuries form on the tailbone, heels, hips, elbows, the back of the head, and under medical equipment such as casts or oxygen masks.
The appearance of these wounds depends on the stage of the pressure injury. In the early stages, pressure injuries appear as areas of reddened skin that do not blanch when pressed. Open sores and deep wounds that expose bone/tissue structures become visible during advanced stages of pressure injuries.
You may not notice pain if you have reduced sensation, even if the wound causes significant tissue damage. You are at risk of pressure ulcers if you are often immobile for extended periods and may suffer from malnutrition, incontinence, fragile skin, and advanced age.
Healing depends on the stage: regular repositioning, moisture control, and good nutrition help. Medical professionals may need to perform surgery or provide specialized wound care for severe cases.
Venous Wounds (Venous Leg Ulcers—VLUs)
-
Chronic Venous Insufficiency (CVI)
Poor blood circulation in the leg veins causes blood to pool, increasing pressure within the veins. The gaiter area above the ankle bone is where these ulcers appear on the inner lower leg. The tissue within these irregular, shallow wounds is red or yellowish. These wounds have moderate to heavy drainage.
The primary symptom of this condition is a dull, aching sensation that typically improves when the legs are elevated. Venous ulcers may also be indicated by swollen tissues, brown or purple skin discoloration, hardened or dry skin, itching, and visible varicose veins.
These wounds require compression therapy to heal. Compression treatment decreases swelling and improves blood circulation. Wound care is just as critical as managing the underlying venous insufficiency.
Recognizing Wounds and Their Symptoms
Timely detection of wounds is essential for successful medical interventions and recovery processes. Patients and their caregivers need to monitor their wounds to identify any worsening of the condition or development of infections.
Key Warning Signs:
- Fresh skin damage, such as sores, ulcers, or blisters, indicates skin breaks. You should check if the wound enlarges or penetrates deeper into the skin. Some wound drainage is normal, but thick discharge with a foul odor and unusual colors like yellow, green, or brown may indicate an infection.
- A persistent foul odor that does not resolve with wound cleaning may indicate infection and should be evaluated by a clinician. A healthy tissue should appear red or pink. Healthcare intervention is necessary for wound areas that appear yellow, black, or brown. Wounds surrounded by red or dark skin may indicate inflammation and poor blood circulation.
- Pain that appears or intensifies suggests either pressure or infection as possible causes. People with diabetes may experience painless wounds, which still indicate infection. Increased temperature around a wound may suggest inflammation or infection, while persistently cold tissue could indicate poor blood flow; overlapping signs may require clinical evaluation.
- New or increased swelling may signal an infection or poor circulation. Severe wound infections may cause systemic symptoms such as fever, chills, red streaks extending from the wound, and, in some cases, nausea.
Diagnosis and Evaluation of Wounds
A complete body assessment and precise diagnosis are essential for effective wound healing. Wound care-trained physical therapists evaluate you by examining your entire body to determine factors that might prevent healing.
During patient history assessment, physical therapists inquire about the origin of the wound, the duration it has been there, past treatments, pain level, fluid drainage, and existing health conditions such as diabetes and heart or vascular diseases. They evaluate:
- The effects of medications
- Your nutrition
- Smoking habits
- Mobility status
- Home support systems
During wound measurement, PTs take precise measurements of wound dimensions while examining for deep, narrow paths known as tunneling and tissue loss beneath the skin surface called undermining.
Examining internal wound tissue helps determine whether it appears healthy, such as when the tissue is red or pink, or presents unhealthy yellow slough or black eschar tissue. The PT also inspects the surrounding skin for infection or damage.
PTs conduct function testing to evaluate your strength, joint movements, balance, and mobility capabilities. These affect healing and the risk of more wounds.
Special Tests
Physical therapists use the Ankle-Brachial Index (ABI) to assess blood flow and detect peripheral artery disease.
Sensation: Testing nerve function, especially in diabetic patients.
Physical therapists should refer patients to physicians when they detect deep infections, persistent wounds, or potentially serious medical conditions.
How Physical Therapy Supports Healing
The primary goal of physical therapy in wound care involves wound healing, functional restoration, and prevention of additional wounds. PTs develop personalized treatment plans based on thoroughly evaluating the patient and their wound.
Customized, Whole-Person Approach
Physical therapists evaluate wound characteristics, including their type, cause, and stage, while assessing your medical records, medications, lifestyle, and support networks. The healing process and care planning incorporate the impact of medical conditions, including diabetes, heart failure, and immune system disorders.
Patient-Centered Goals
Therapists collaborate with patients and their caregivers to establish essential treatment plans, which may involve pain reduction, improved mobility, and enhanced life quality.
Education and motivation are critical. A PT helps you know your medical situation and gives you control over the treatment process. A successful wound management strategy requires you, your caregiver, and your therapist to collaborate.
Physical Therapy for Wound Healing
Patient and Caregiver Education
Your physical therapist will instruct you and your caregiver about proper wound care techniques and how to detect infection symptoms while demonstrating safe body movements to shield the skin. Physical therapists will show you methods for reducing pressure on wounds and proper bed-to-chair transfer techniques.
Strength and Mobility Exercises
Physical therapists create individualized exercise plans that enhance blood flow and minimize swelling to stop new injuries from occurring. The treatment plan incorporates stretching exercises, balance training, and low-impact exercises that include walking and cycling.
Wound Care Techniques
Therapists select the right dressings to maintain moisture in the wound and provide protection.
Advanced Therapies
The healing process can be accelerated through electrical stimulation, ultrasound therapy, and compression bandaging techniques, which PTs often employ. Total contact casts, usually applied by wound specialists, help offload pressure on foot ulcers and promote healing.
These applied techniques accelerate wound healing while improving patient mobility and quality of life.
Adaptive Equipment and Environment Modification
Physical therapists assist wound patients by recommending equipment and home modifications that minimize skin pressure, protect tissue integrity, and enhance comfort and functionality.
Support Surfaces
Special mattresses and cushions help prevent pressure injuries by evenly distributing body weight. Foam and gel surfaces are static and conform to the body to help distribute pressure, while air overlays may offer limited dynamic support depending on their design.
The pressure distribution on your body occurs through air movement in dynamic surfaces such as alternating pressure mattresses. Support surfaces are chosen based on risk level, injury location, mobility, and body weight.
Shoes and Offloading
People with diabetes or foot wounds should wear proper shoes because they protect their feet. Therapeutic shoes minimize the pressure and friction on the feet.
Your ulcer healing will improve with offloading devices such as total contact casts, walker boots, and specialized shoes that reduce pressure on the affected areas.
Ongoing Monitoring
Therapists monitor wound healing by taking measurements of the wound area and inspecting the skin condition. The therapist will modify your dressing materials, treatment protocols, and equipment whenever necessary.
Warning Signs that Require Further Assistance
Contact your doctor immediately if you experience:
- New or worsening pain
- Redness
- Swelling
- Pus
- Fever
- Bad smell
- Bleeding
- Sudden skin changes.
The symptoms might indicate either infection or circulation problems.
Choosing the Right Physical Therapist
A physical therapist specializing in wound care provides better outcomes for healing patients. Therapists possess universal training. However, those with Wound Care Specialist (WCS) or Certified Wound Specialist (CWS) certifications demonstrate specialized competencies. Inquire about their background in wound care and their ongoing education programs.
Find Wound Care Services Near Me
Wounds caused by diabetes, poor circulation, and prolonged pressure can lead to serious complications that interfere with daily life. Fortunately, physical therapy can prevent and treat these wounds. A skilled physical therapist uses personalized care and advanced treatments to improve healing, reduce complications, and help you stay active and independent. Early intervention is key to avoiding severe complications. Do not wait for wounds to worsen. If you are in Las Vegas, schedule your personalized evaluation with Suarez Physical Therapy at 702-368-6778 today and take the first step toward recovery.